Retic count in sickle cell – Reticulocyte count takes center stage in sickle cell disease, offering valuable insights into disease severity and response to treatment. This comprehensive guide delves into the concept of reticulocytes, their significance in evaluating erythropoiesis, and their clinical interpretation in the context of sickle cell disease.
Delving deeper, we explore the methods used for reticulocyte counting, including manual and automated techniques. We discuss the principles and accuracy of each method, providing a clear understanding of their applications.
Reticulocyte Count Definition: Retic Count In Sickle Cell
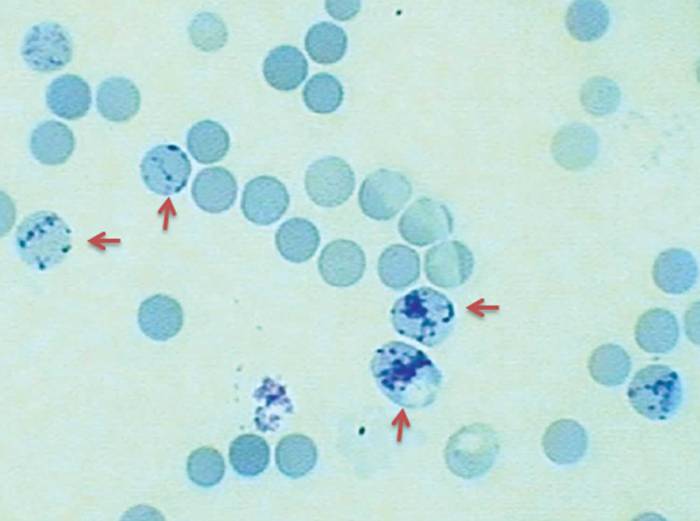
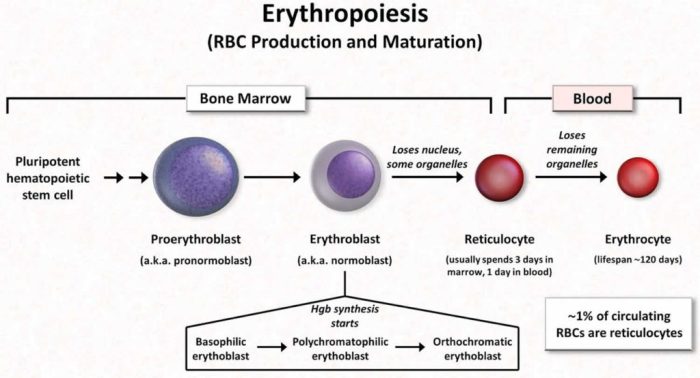
Reticulocytes are immature red blood cells that are released from the bone marrow into the bloodstream. They are characterized by the presence of RNA remnants, which give them a distinctive reticular or net-like appearance when stained with a special dye called new methylene blue.
The reticulocyte count is a measure of the number of reticulocytes in the blood. It is used to assess the rate of erythropoiesis, or red blood cell production. A normal reticulocyte count is between 0.5% and 1.5% of all red blood cells.
Significance of Reticulocyte Count
The reticulocyte count is a valuable tool for evaluating erythropoiesis. A high reticulocyte count indicates that the bone marrow is producing red blood cells at an increased rate, which may be in response to anemia or blood loss. A low reticulocyte count, on the other hand, may indicate that the bone marrow is not producing enough red blood cells, which can lead to anemia.
Reticulocyte Count in Sickle Cell Disease
Reticulocyte count plays a crucial role in assessing disease severity and treatment response in sickle cell disease. It reflects the bone marrow’s ability to produce red blood cells to compensate for the destruction of sickle-shaped red blood cells.
Characteristic Reticulocyte Count
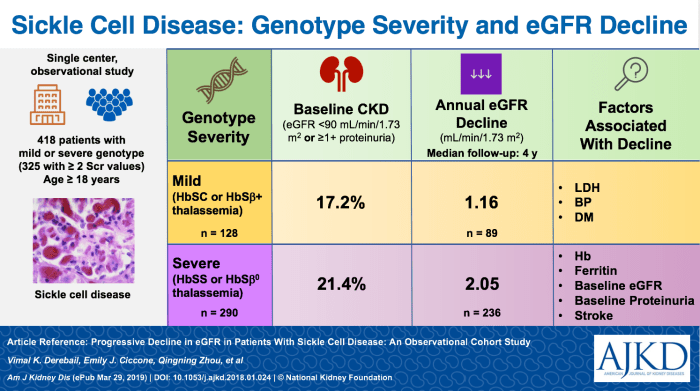
In sickle cell disease, the reticulocyte count is typically elevated, indicating increased red blood cell production. This elevation can vary depending on the severity of the disease and the effectiveness of treatment.
Disease Severity and Treatment Response
A high reticulocyte count often correlates with more severe disease, as it suggests that the bone marrow is working harder to replace the damaged red blood cells. Conversely, a lower reticulocyte count may indicate milder disease or a positive response to treatment, as the bone marrow is not under as much pressure to produce new red blood cells.
Methods for Reticulocyte Counting
Reticulocyte counting is essential in assessing erythropoietic activity in sickle cell disease. There are two main methods for reticulocyte counting: manual and automated.
Manual Method
The manual method involves staining a blood smear with a supravital stain, such as brilliant cresyl blue, and counting the reticulocytes under a microscope. Reticulocytes appear as blue-stained cells with a reticular network, while mature red blood cells appear as non-stained cells.
The manual method is relatively inexpensive and widely available. However, it is time-consuming and requires a skilled technician to accurately identify reticulocytes.
Automated Method
The automated method uses flow cytometry to count reticulocytes. Flow cytometry involves passing a stream of stained cells through a laser beam and measuring the light scattering and fluorescence of each cell. Reticulocytes have a higher RNA content than mature red blood cells, which results in increased fluorescence.
The automated method is more rapid and objective than the manual method. However, it is more expensive and requires specialized equipment.
Tracking retic count in sickle cell can be a challenge, but don’t worry! Check out this awesome i am someone who worksheet for guidance. It’s like a personal trainer for your retic count, helping you understand its importance and monitor it effectively.
Clinical Interpretation of Reticulocyte Count
The reticulocyte count provides valuable insights into the erythropoietic activity in the bone marrow. Understanding the normal range and interpreting elevated or decreased reticulocyte counts is crucial for assessing the clinical status of individuals with sickle cell disease.
Normal Range
In healthy individuals, the normal range of reticulocyte count is typically between 0.5% and 1.5% of the total red blood cells. This range reflects a balance between the production and maturation of red blood cells in the bone marrow.
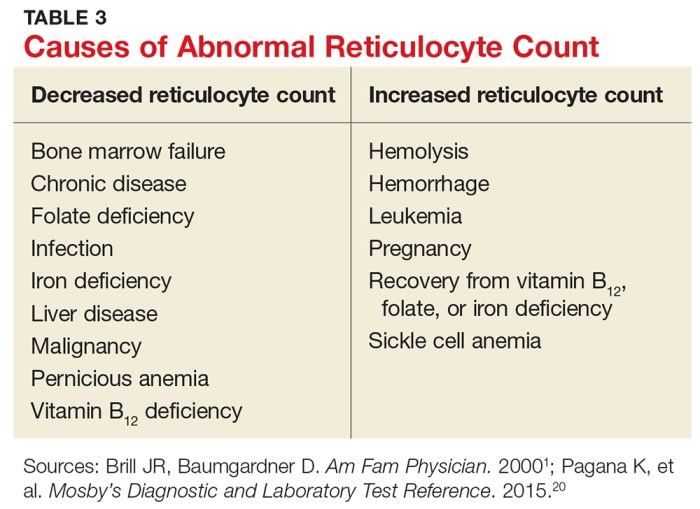
Elevated Reticulocyte Count
An elevated reticulocyte count, known as reticulocytosis, indicates increased erythropoietic activity in the bone marrow. In sickle cell disease, reticulocytosis is often associated with hemolytic episodes or acute complications, such as vaso-occlusive crises or infections. It reflects the body’s attempt to compensate for the increased destruction of red blood cells.
Decreased Reticulocyte Count
A decreased reticulocyte count, known as reticulocytopenia, suggests impaired erythropoiesis in the bone marrow. In sickle cell disease, reticulocytopenia can indicate bone marrow failure, aplastic crisis, or other factors that suppress red blood cell production. It can lead to anemia and further complications.
Role of Reticulocyte Count in Monitoring Treatment
Reticulocyte count plays a crucial role in monitoring the effectiveness of treatments for sickle cell disease. It provides valuable information about the response of the bone marrow to therapy and the overall health of the patient.
Implications of Persistent Reticulocytosis
Persistent reticulocytosis, a condition characterized by an elevated reticulocyte count, can indicate:
- Inadequate response to treatment
- Hemolysis or destruction of red blood cells
- Bone marrow suppression
Implications of Persistent Reticulocytopenia
On the other hand, persistent reticulocytopenia, or a low reticulocyte count, may suggest:
- Effective suppression of red blood cell production
- Bone marrow failure
- Nutritional deficiencies
Limitations and Considerations
While the reticulocyte count is a valuable tool in sickle cell disease, it has certain limitations and factors that can affect its accuracy.
Factors that can influence the reticulocyte count include:
Coexisting Conditions, Retic count in sickle cell
- Iron deficiency:Iron is essential for hemoglobin production, and its deficiency can lead to decreased reticulocyte production.
- Infection:Infections can cause an increase in reticulocyte production, as the body attempts to replenish red blood cells destroyed by the infection.
- Splenomegaly:An enlarged spleen can trap reticulocytes, resulting in a falsely low reticulocyte count.
Medications
- Hydroxyurea:Hydroxyurea, a medication used to treat sickle cell disease, can increase reticulocyte production.
- Antiretroviral therapy:Antiretroviral drugs used to treat HIV can also increase reticulocyte production.
Essential Questionnaire
What is the normal range of reticulocyte count?
The normal range for reticulocyte count in healthy individuals is typically between 0.5% and 1.5%.
How does reticulocyte count reflect disease severity in sickle cell disease?
Elevated reticulocyte count often indicates increased erythropoiesis, which may be a compensatory response to hemolysis or ineffective erythropoiesis. Conversely, decreased reticulocyte count suggests suppressed bone marrow activity or impaired erythroid maturation.
What are the limitations of reticulocyte count as a diagnostic tool?
Reticulocyte count can be affected by factors such as coexisting conditions, medications, and blood transfusions. Therefore, it should be interpreted in conjunction with other clinical findings and laboratory tests.